Express Scripts Prior Authorization Form Printable
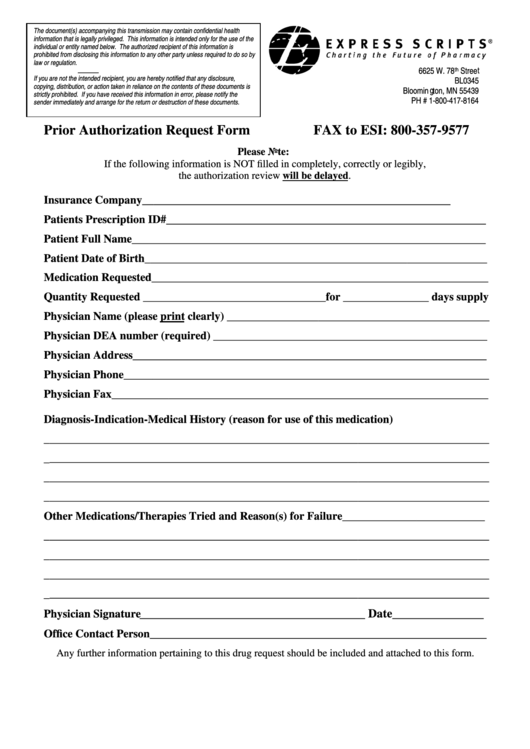
Express Scripts Prior Authorization Form Printable - Your medical necessity approval will apply at network pharmacies. Requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. To be used only for prescriptions which are to be filed through. Easily fill out pdf blank, edit, and sign them. Certain plans and situations may require additional information beyond what is specifically. This form is based on express scripts standard criteria and may not be applicable to all patients; Certain plans and situations may require additional information beyond what is specifically. The evicore ® by evernorth portal lets you manage prescription drug epas for patients with express scripts pharmacy benefits. Prior authorization (pa) also known as a “coverage review,” this is a process health plans might use to decide if your prescribed medicine will be covered. Any plan member who is prescribed a medication that requires prior authorization needs to complete and submit this form. Tricare prior authorization request form for compounded medications to be completed and signed by the prescriber. Only a treating physician can determine what. This fax form is based on express scripts standard criteria; 44 express scripts prior authorization form templates are. Based upon each patient’s prescription plan, additional. To be used only for prescriptions which are to be filed through. Your medical necessity approval will apply at network pharmacies. Ask your doctor to either call express scripts to request a coverage review or to prescribe an alternative medication that’s covered by your plan. Get your written prescriptions to us by using our mail order form. Tricare prior authorization request form for ozempic, mounjaro. After express scripts receives a prior. Save or instantly send your ready. Download and print the form for your drug. Up to $40 cash back complete express scripts prior authorization form online with us legal forms. Your prescriber may use the attached. 44 express scripts prior authorization form templates are. Any fees related to the completion of this form are the. Up to $40 cash back complete express scripts prior authorization form online with us legal forms. This form is based on express scripts standard criteria and may not be applicable to all patients; After express scripts receives a prior. To be used only for prescriptions which are to be filed through. This form is based on express scripts standard criteria and may not be applicable to all patients; Requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. Download and print the form for your drug. This form is based on express. We can't complete your request at this time. Plans use this to help control costs. This form is based on express scripts standard criteria and may not be applicable to all patients; Tricare prior authorization request form for compounded medications to be completed and signed by the prescriber. This form is based on express scripts standard criteria and may not. Find tricare claims forms, our medical questionnaire, and other important documents all collected in one convenient place. Prior authorization (pa) also known as a “coverage review,” this is a process health plans might use to decide if your prescribed medicine will be covered. Tricare prior authorization request form for ozempic, mounjaro. Trying to access your account? 44 express scripts prior. Certain plans and situations may require additional information beyond what is specifically. Plans use this to help control costs. To be used only for prescriptions which are to be. Get your written prescriptions to us by using our mail order form. Any plan member who is prescribed a medication that requires prior authorization needs to complete and submit this form. Certain plans and situations may require additional information beyond what is specifically. Plans use this to help control costs. Any plan member who is prescribed a medication that requires prior authorization needs to complete and submit this form. This form is based on express scripts standard criteria and may not be applicable to all patients; Easily fill out pdf blank,. Plans use this to help control costs. Certain plans and situations may require additional information. Any fees related to the completion of this form are the. This form is based on express scripts standard criteria and may not be applicable to all patients; To be used only for prescriptions which are to be filed through. Save or instantly send your ready. Up to $40 cash back complete express scripts prior authorization form online with us legal forms. Give the form to your provider to complete and send back to express scripts. This form is based on express scripts standard criteria and may not be applicable to all patients; After express scripts receives a prior. Up to $40 cash back complete express scripts prior authorization form online with us legal forms. Ask your doctor to either call express scripts to request a coverage review or to prescribe an alternative medication that’s covered by your plan. Plans use this to help control costs. Prior authorization of benefits is not the practice of medicine or a substitute. Easily fill out pdf blank, edit, and sign them. Up to $40 cash back complete express scripts prior authorization form online with us legal forms. Find tricare claims forms, our medical questionnaire, and other important documents all collected in one convenient place. Plans use this to help control costs. Your prescriber may use the attached. To be used only for prescriptions which are to be filed through. Based upon each patient’s prescription plan, additional. The evicore ® by evernorth portal lets you manage prescription drug epas for patients with express scripts pharmacy benefits. After express scripts receives a prior. If this problem continues, please call the number on the back of your member id card. 44 express scripts prior authorization form templates are collected for any of. Give the form to your provider to complete and send back to express scripts. Ask your doctor to either call express scripts to request a coverage review or to prescribe an alternative medication that’s covered by your plan. Certain plans and situations may require additional information beyond what is specifically. This fax form is based on express scripts standard criteria; Your medical necessity approval will apply at network pharmacies.Prior Authorization Request Form printable pdf download
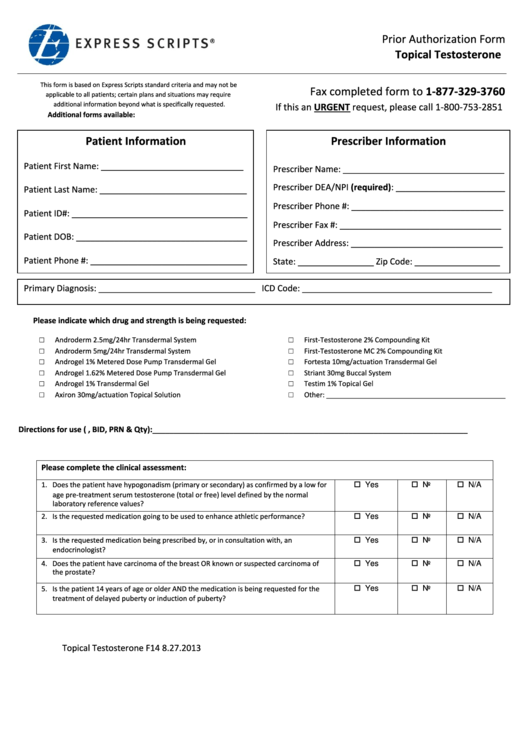
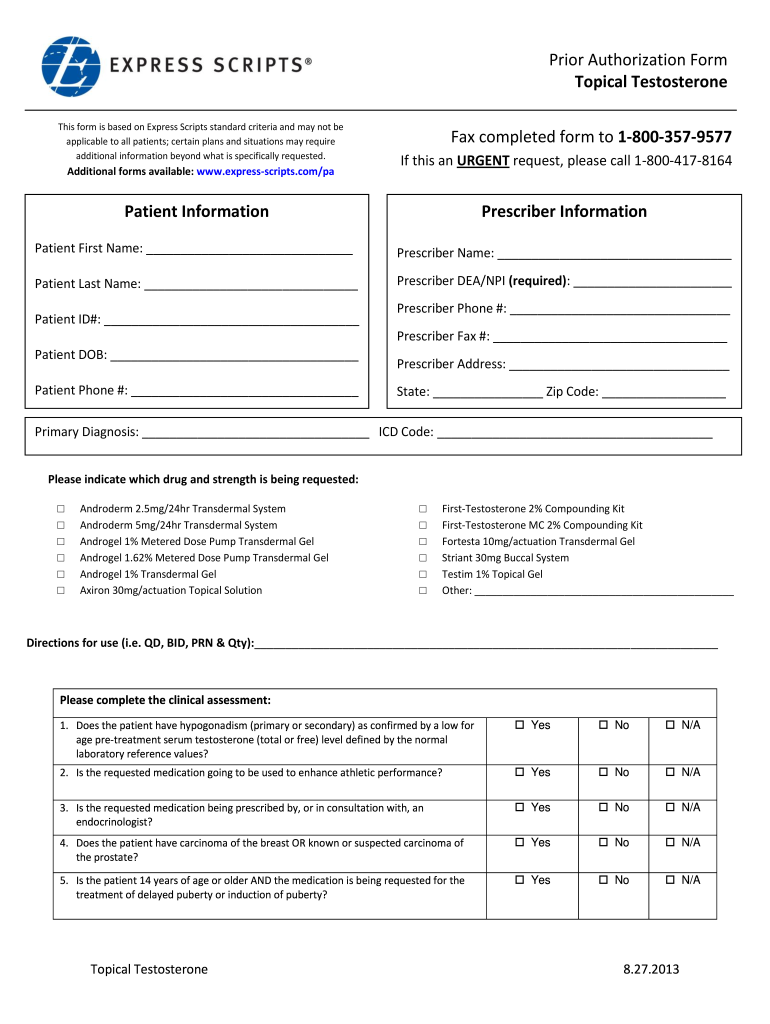
Express Scripts Prior Authorization Form Topical Testosterone
Express Scripts Prior Authorization Form 2023 Pdf Printable Forms
Fillable Online Fillable Online Tricare express scripts prior
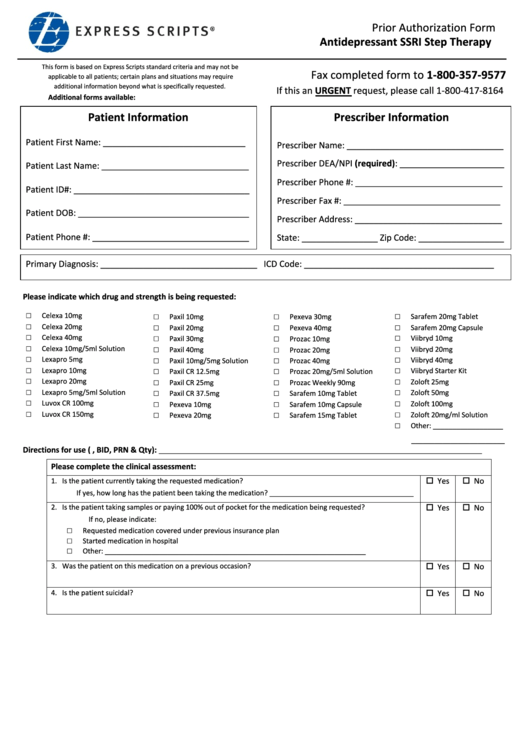
Prior Authorization Form Antidepressant Express Scripts printable pdf
Free Express Scripts Prior (Rx) Authorization Form PDF eForms
Express Scripts Prior Authorization 20132024 Form Fill Out and Sign
Fillable Online Free Express Scripts Prior Prescription (Rx
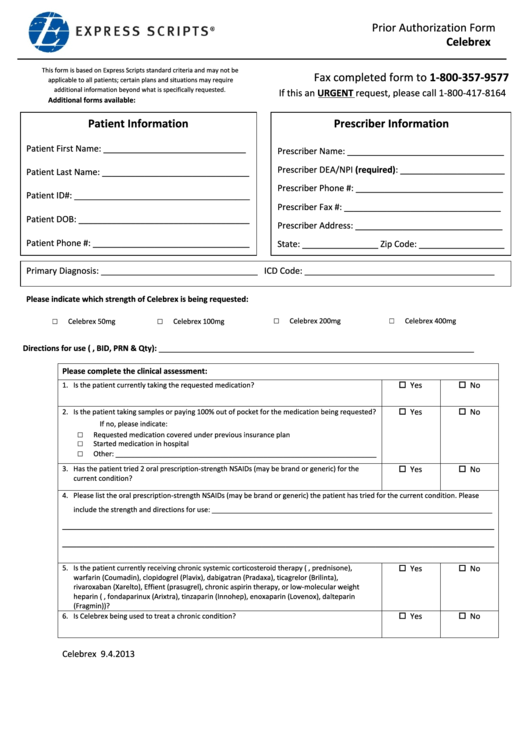
Express Scripts Prior Authorization Celebrex printable pdf download
SCAN Health Plan Express Scripts Prior Authorization 20212022 Fill
This Form Is Based On Express Scripts Standard Criteria And May Not Be Applicable To All Patients;
Certain Plans And Situations May Require Additional Information Beyond What Is Specifically.
Prior Authorization Of Benefits Is Not The Practice Of Medicine Or A Substitute For The Independent Medical Judgment Of A Treating Physician.
Certain Plans And Situations May Require Additional Information Beyond What Is Specifically.
Related Post: