Cvs Caremark Appeal Form Printable
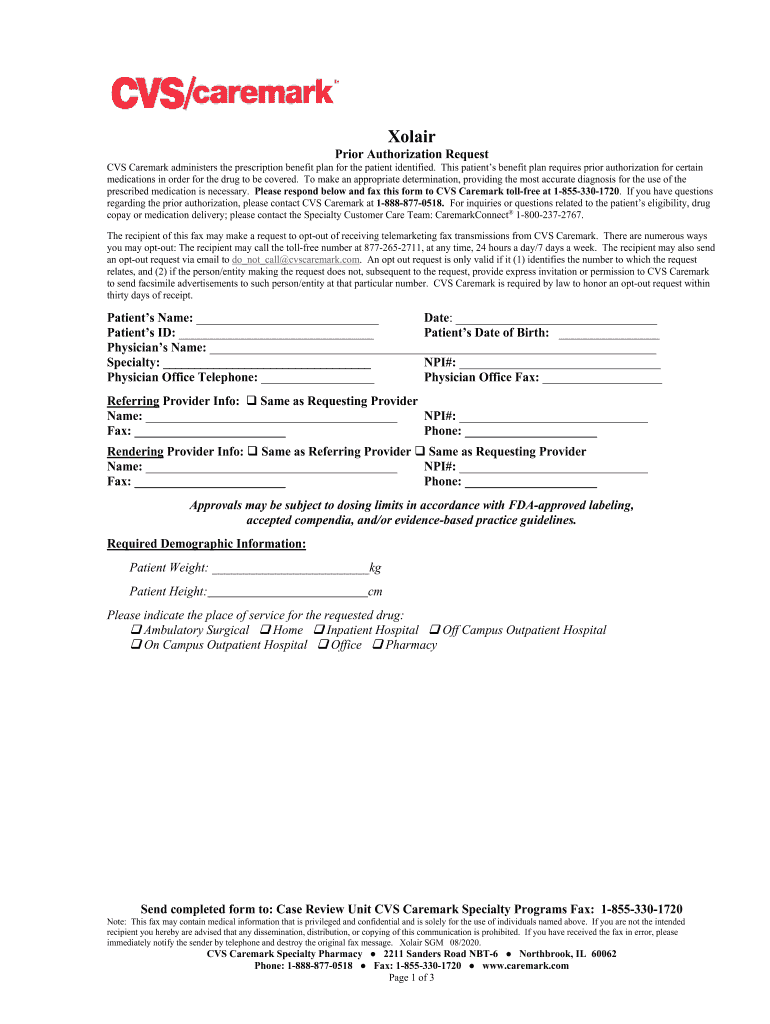
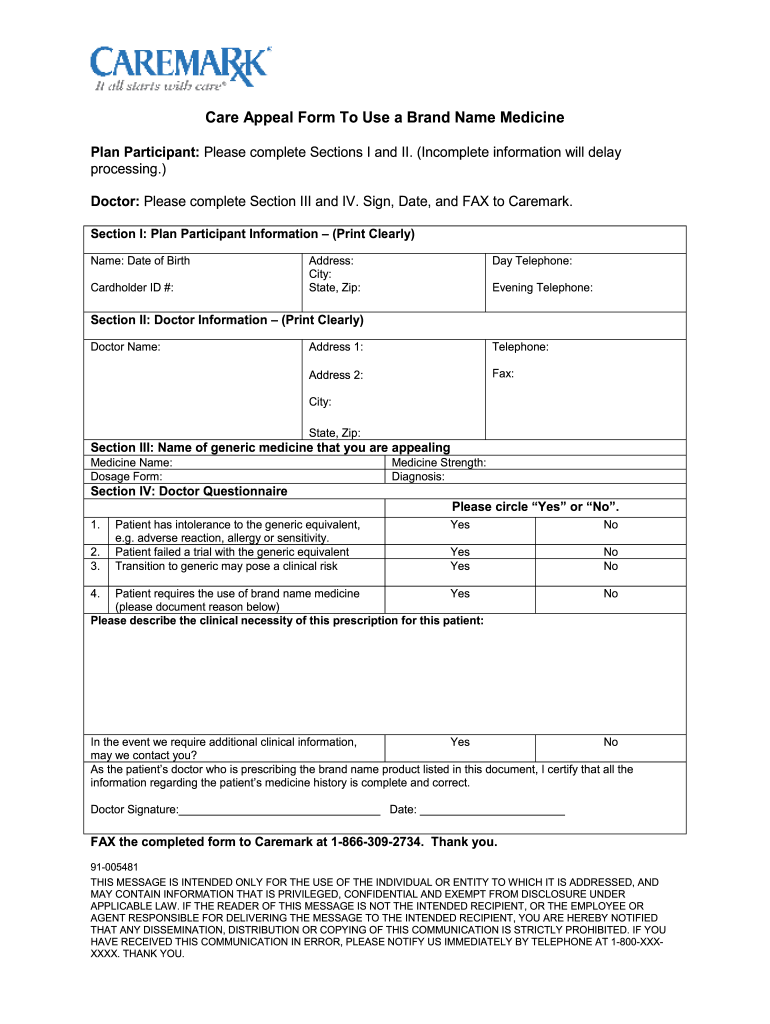
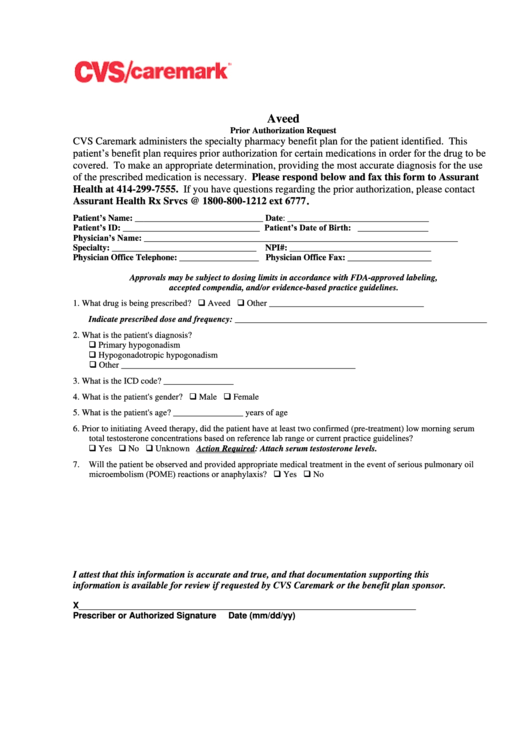
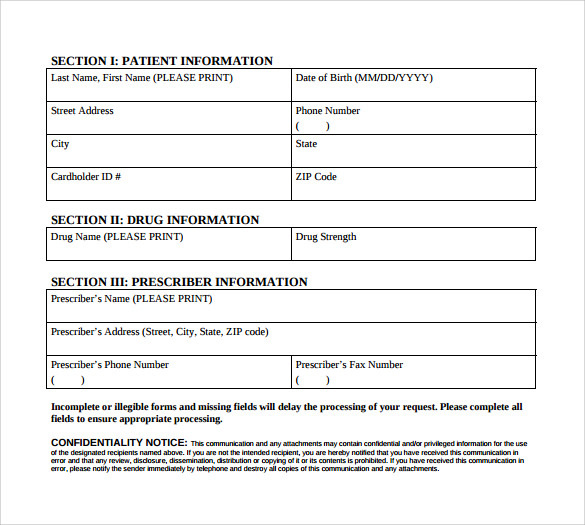
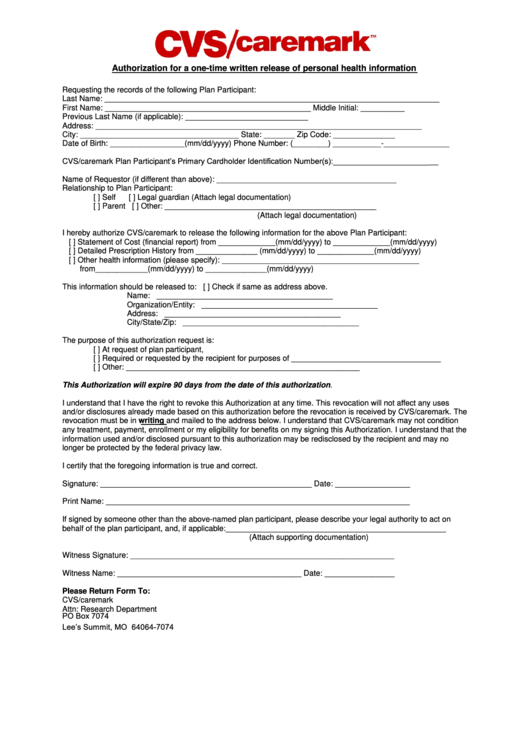
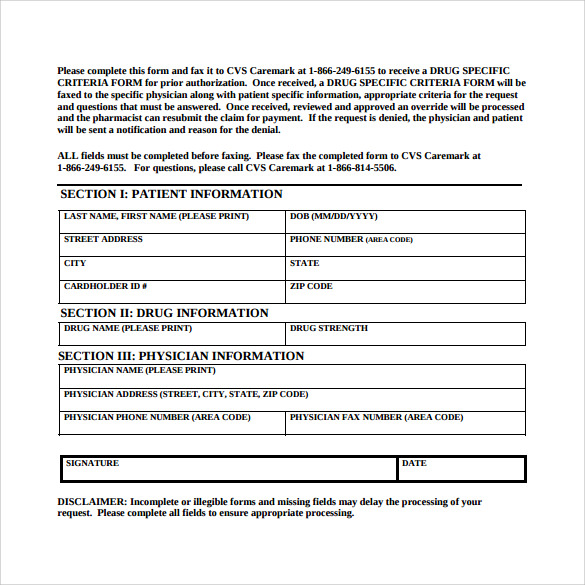
Cvs Caremark Appeal Form Printable - To manage your prescriptions, sign in or register • a clear statement that the communication is intended to. It contains instructions on how to submit a letter of medical necessity. If your drug is denied, both you and your doctor will receive. Expedited appeal requests can be made by phone 24 hours a day, 7 days a week. Print plan forms download a form to start a new mail order prescription. Appeal requests must be received within 180 days of receipt of the adverse determination letter. A cvs/caremark prior authorization form is used by a medical office when requesting coverage for a cvs/caremark plan member's prescription. To manage your prescriptions, sign in or register Print plan forms download a form to start a new mail order prescription. If your drug is denied, both you and your doctor will receive. Expedited appeal requests can be made by phone 24 hours a day, 7 days a week. Has extensive disease, dermatophyte folliculitis is present, did not respond to topical. Find out how to request prior authorization for certain drugs and services covered by cvs caremark. Your prescriber may ask us for an appeal on your behalf. A physician will need to. Find pa forms for physicians to request coverage for prescriptions. Once an appeal is received, the appeal and all supporting documentation are reviewed and. If you want another individual (such as a. Is the request for treatment of tinea corporis or tinea cruris in a patient who meets any of the following: • a clear statement that the communication is intended to. This information is provided in prior. Find out how to request prior authorization for certain drugs and services covered by cvs caremark. Print plan forms download a form to start a new mail order prescription. If your drug is denied, both you and your doctor will receive. Expedited appeal requests can be made by phone. Your appeal may require immediate action if a delay in treatment could significantly increase the risk to your health or the ability to regain maximum function or cause severe pain. Has extensive disease, dermatophyte folliculitis is present, did not respond to topical. It provides necessary instructions for submitting a letter of. Cvs. To manage your prescriptions, sign in or register To manage your prescriptions, sign in or register Print plan forms download a form to start a new mail order prescription. • a clear statement that the communication is intended to. Your appeal may require immediate action if a delay in treatment could significantly increase the risk to your health or the. Contact us to learn how to name a representative. Your appeal may require immediate action if a delay in treatment could significantly increase the risk to your health or the ability to regain maximum function or cause severe pain. The cvs caremark mobile app is ready to help you quickly refill a prescription, find a network pharmacy, check drug costs,. Your first appeal request must be submitted to the claims administrator within 180 days after you receive the claim denial. Appeal requests must be received within 180 days of receipt of the adverse determination letter. If you want another individual (such as a. To manage your prescriptions, sign in or register Print plan forms download a form to start a. Find pa forms for physicians to request coverage for prescriptions. To manage your prescriptions, sign in or register Is the request for treatment of tinea corporis or tinea cruris in a patient who meets any of the following: If you want another individual (such as a. Find out how to request prior authorization for certain drugs and services covered by. Your appeal may require immediate action if a delay in treatment could significantly increase the risk to your health or the ability to regain maximum function or cause severe pain. Cvs caremark appeal process guide. Your first appeal request must be submitted to the claims administrator within 180 days after you receive the claim denial. Expedited appeal requests can be. Your first appeal request must be submitted to the claims administrator within 180 days after you receive the claim denial. Cvs caremark appeal process guide. Your appeal may require immediate action if a delay in treatment could significantly increase the risk to your health or the ability to regain maximum function or cause severe pain. Download and print this form. Download and print this form to request a coverage determination for a prescription drug from cvs/caremark. A physician will need to. Is the request for treatment of tinea corporis or tinea cruris in a patient who meets any of the following: This document outlines the appeal process for medication denials with cvs caremark. This file outlines the appeal process for. A cvs/caremark prior authorization form is used by a medical office when requesting coverage for a cvs/caremark plan member's prescription. We want to make sure you get the most out of. This document outlines the appeal process for medication denials with cvs caremark. Expedited appeal requests can be made by phone 24 hours a day, 7 days a week. Print. Find out how to request prior authorization for certain drugs and services covered by cvs caremark. Expedited appeal requests can be made by phone. • a clear statement that the communication is intended to. If your drug is denied, both you and your doctor will receive. We want to make sure you get the most out of. It contains instructions on how to submit a letter of medical necessity. If you want another individual (such as a. Once an appeal is received, the appeal and all supporting documentation are reviewed and. Your first appeal request must be submitted to the claims administrator within 180 days after you receive the claim denial. To manage your prescriptions, sign in or register Print plan forms download a form to start a new mail order prescription. A physician will need to. Cvs caremark appeal process guide. To manage your prescriptions, sign in or register This document outlines the appeal process for medication denials with cvs caremark. Download and print this form to request a coverage determination for a prescription drug from cvs/caremark.Cvs caremark wegovy prior authorization criteria Fill out & sign
Cvs Caremark Appeal Form Edit & Share airSlate SignNow
Cvs Aveed Prior Authorization Request Form printable pdf download
9+ Sample Caremark Prior Authorization Forms Sample Templates
Cvs Pharmacy Prior Authorization Form
Fillable Online HMSA Prior Authorization Request CVS Caremark Fax
Fillable Online CVS Caremark Prior Authorization Forms Fax Email Print
FREE 8+ Sample Caremark Prior Authorization Forms in PDF
Fillable Online Free CVS/Caremark Prior (Rx) Authorization Form PDF
Fillable Online Cvs Caremark Prior Authorization Form For . Cvs
Appeal Requests Must Be Received Within 180 Days Of Receipt Of The Adverse Determination Letter.
This File Outlines The Appeal Process For Cvs Caremark.
Your Appeal May Require Immediate Action If A Delay In Treatment Could Significantly Increase The Risk To Your Health Or The Ability To Regain Maximum Function Or Cause Severe Pain.
This Information Is Provided In Prior.
Related Post: